The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Brain Structure Alterations Associated with Substance Use Disorder
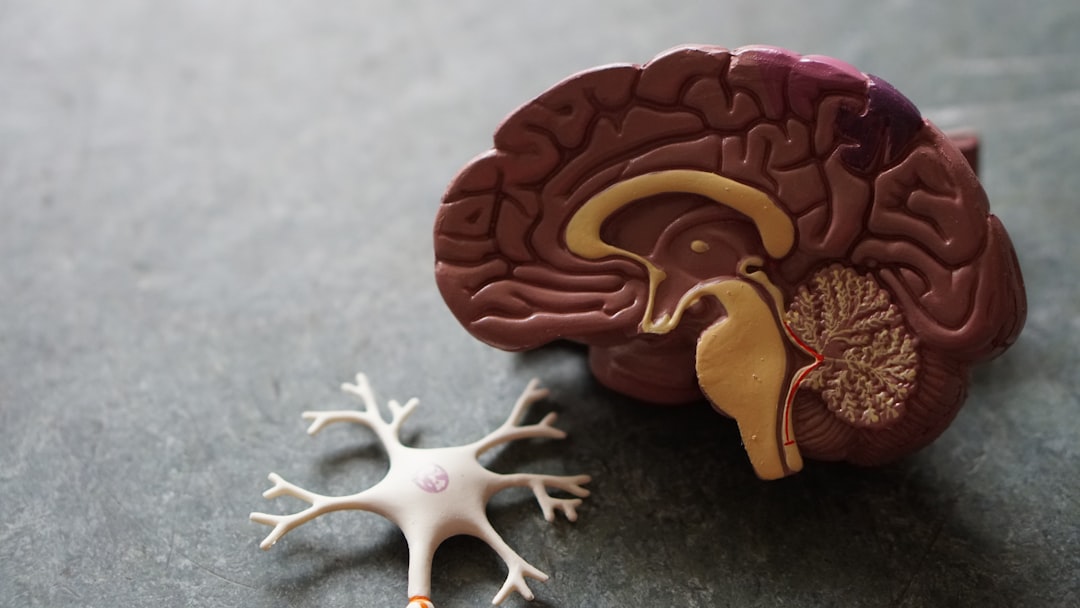
Substance Use Disorder (SUD) is characterized by substantial alterations in brain structure, leading to challenges in treatment. Individuals with SUD commonly display changes in both gray and white matter, particularly within brain regions involved in reward processing, impulse control, and decision-making. The prefrontal cortex, a key area for evaluating risks and regulating actions, frequently exhibits marked changes in SUD. These brain alterations can be further aggravated when substance use begins during adolescence, potentially increasing the risk of future addiction. Recognizing the unique structural changes linked to specific substances is essential for developing tailored therapies that effectively address individual needs. This is a complex field, and the specific structural changes associated with different substances are not always easily identified. However, the more we learn, the better the prospects of guiding therapies to specific areas of brain alteration that might provide a better chance of long-term recovery.
Substance use disorders are increasingly understood as conditions that significantly reshape the brain's physical structure, with particular impact on areas vital for decision-making and impulse control. For instance, research suggests that regions like the prefrontal cortex, a key player in executive function, experience reductions in gray matter volume in individuals with SUD.
The amygdala, a brain structure central to emotional processing, also appears susceptible to the effects of prolonged substance use. Shrinkage of this region could potentially amplify feelings of anxiety and stress, a common feature in individuals struggling with SUD. It remains to be seen whether these structural changes directly contribute to these emotional responses, or are merely associated with SUD.
Beyond changes in gray matter, substance use has been shown to disrupt the brain's white matter, the network of fibers that connect different regions. Reduced integrity and density in these connections can disrupt efficient information flow between critical brain regions, potentially affecting cognition and emotional regulation. This area needs further research, as current evidence is not conclusive on its role in SUD.
Investigations using neuroimaging have unveiled alterations in brain activity patterns, particularly in the basal ganglia. This network, strongly tied to reward processing, shows increased activation and connectivity in people with SUD, potentially contributing to heightened cravings and a higher likelihood of relapse. More research needs to be performed to confirm this connection.
Further complicating the picture, the hippocampus, crucial for memory formation and learning, often undergoes structural changes in the context of SUD. These changes may contribute to impairments in forming new memories and difficulties learning from past experiences related to substance use, especially as it pertains to addiction. This, if confirmed, might be an area to focus on with tailored treatments.
The brain's capacity for neuroplasticity, or the ability to reshape itself, comes into play with substance use. The brain adapts to the presence of drugs, leading to phenomena such as tolerance and a persistent drive to seek substances even when faced with negative consequences. Further research into the individual brain's ability to undergo neuroplasticity in relation to drug use might yield new therapeutic options.
Some substances, such as alcohol, have shown evidence of causing neurodegeneration, particularly in the frontal lobes. This could exacerbate the poor decision-making and risky behaviors commonly associated with SUD, a critical area for ongoing study.
The impact of SUD on brain structure is not uniform across all substances. Different drugs can lead to distinct patterns of structural changes, suggesting that treatment approaches tailored to the specific substance of abuse may be more effective. Further development of individualized treatments based on this type of data could help those suffering from SUD.
Achieving long-term abstinence from drugs doesn't necessarily equate to a complete reversal of brain structural alterations. Some changes can persist for years after cessation of drug use, emphasizing the importance of continued therapy and support to aid in recovery. Further study is needed into the efficacy of extended treatment strategies for SUD.
Advances in neuroimaging technologies have offered a clearer view of how substance use alters the brain over time. These insights highlight the significance of early intervention, aiming to minimize the long-term structural damage that can result from extended substance use. More research needs to be performed on the ability to determine SUD risk and initiate early treatments.
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Genetic and Environmental Factors Influencing SUD Development
The emergence of Substance Use Disorders (SUDs) is a complex process shaped by a combination of genetic and environmental factors. Genetic influences play a significant role, with studies suggesting that genetics account for a substantial portion—estimated at 40-70%—of the variability in addictive behaviors. Recent advancements in genomics, specifically through genome-wide association studies, have begun to identify particular genes associated with increased risk of SUDs, providing a more detailed understanding of the genetic basis of addiction. However, the picture is far more intricate than simply genetics. Environmental factors exert a powerful influence as well, interacting with genetic predisposition to shape the likelihood of SUD development. These environmental influences include a wide range of elements, such as the availability of substances, the social environment (including peer and family dynamics), cultural norms, stress levels, and socioeconomic factors. Understanding this intricate interplay between genes and environment is essential for creating effective interventions and prevention strategies for SUDs. Recognizing that addiction likely arises from the complex interplay of many genes, each contributing a small degree of risk, calls for a multi-faceted approach that accounts for both inherited susceptibility and the environmental context. It also underscores the importance of early intervention, as the genetic predisposition to SUD can influence brain development even before substance use begins. Ultimately, acknowledging the multifaceted nature of SUD etiology is critical for crafting more effective strategies to prevent and treat these disorders.
Substance use disorders (SUDs) are a complex interplay of inherited traits and environmental factors, with genetic contributions estimated to influence 40-70% of the variability in addictive behaviors. While there's a growing understanding of the genetic basis for addiction, much of it remains unclear. Recent genetic research, particularly genome-wide association studies (GWAS), has started to pinpoint specific genetic markers linked to SUDs, shedding light on the molecular mechanisms behind addiction vulnerability.
These genetic underpinnings, coupled with an individual's age of initial substance use, personality traits, and past psychological experiences, create a unique neurobiological landscape that interacts with the environment. Environmental factors—like the ready availability of drugs, family and peer influences, cultural norms, exposure to stress, and socio-economic conditions—play a significant role in shaping an individual's risk of developing an SUD.
Essentially, addiction appears to be a polygenic disorder, where numerous genes, each with a small contribution, combine to increase susceptibility. Intriguingly, this genetic predisposition can affect brain development from very early on, even before substance use begins, implying a potential importance of extremely early interventions to prevent SUD. This highlights the potential impact of genetics on an individual's brain structure and function from a very early age, potentially influencing the development of SUD.
There's a wide range of genetic risks for SUDs. Family and twin studies demonstrate the clear influence of genetics, with similar genetic risk factors observed across various substance types. This suggests that there are shared biological pathways that underlie addiction to different substances, and that a broader perspective is needed to address the core issue and prevent future relapses.
It's important to emphasize the role of psychological factors in individual vulnerability to SUDs. An individual's life history, personality traits, and psychological makeup are all significant factors that can influence their susceptibility. While these factors seem to be connected to genetic traits in some cases, they still may present unique challenges for certain individuals.
Because SUDs stem from a combination of genetic and environmental factors, adopting a multifaceted approach to prevention and treatment is critical. Understanding the specific interactions between an individual's genetic background and their unique environmental experiences holds promise for developing more customized prevention and treatment programs. The complexity of SUD development suggests that tailoring treatments to address the diverse combination of factors affecting each individual is likely to be the most effective approach.
The risk for SUD varies considerably between individuals, which can be attributed to a complex interplay of genetic and environmental factors. Some individuals might have a stronger genetic predisposition toward SUD, while others might have experienced traumatic childhoods that make them more vulnerable. These factors might interact or might act as independent triggers in the development of SUD. It's becoming increasingly clear that understanding this interaction is critical for developing the most effective therapies and strategies for prevention.
Psychological factors, such as individual experiences and personality, can significantly impact an individual's likelihood of developing SUD. These factors are likely influenced by a person's genetic background, but are also influenced by a myriad of specific environmental influences. This makes it difficult to design effective interventions in some cases, because there is not a clear understanding of exactly how these factors interact to produce an SUD.
The multifactorial nature of SUDs underscores the importance of a multidimensional approach to treatment. By taking into account an individual's unique genetic make-up and life experiences, we can craft more effective prevention strategies and treatment plans. It is crucial for prevention and treatment strategies to recognize and effectively address the dynamic relationship between genetic risk, environmental triggers, and the individual's psychological landscape. This research has the potential to significantly impact treatment of SUDs and hopefully lead to higher rates of long-term recovery.
Ongoing research continues to unravel the intricacies of SUD development, offering the potential for increasingly refined interventions that cater to individual differences. By understanding the dynamic interplay between genetic and environmental influences, we can work towards developing more effective prevention and treatment strategies for SUD, ultimately striving to improve recovery outcomes and minimize the risk of relapse. This area of research has huge potential to improve outcomes and create a more humane and effective approach to SUD treatment.
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Comorbidity of Substance Use Disorders and Mental Illness
The frequent co-occurrence of substance use disorders (SUD) and various mental health conditions presents a substantial challenge in both identifying the specific disorder and creating effective treatment plans. A significant portion, roughly 41%, of individuals dealing with SUD also have a concurrent mental illness, making the clinical picture quite complex and potentially reducing the effectiveness of any treatment. Depression, specifically, is quite common among those with SUD, emphasizing the strong connection between these conditions and the need for treatment approaches that address both issues simultaneously. The reasons for this overlap are complex and may be based on shared biological systems. Gaining a thorough understanding of the neurobiological mechanisms that drive this comorbidity is of critical importance, as it could lead to therapies that are more targeted and effective. The added difficulty of dealing with these co-occurring conditions underscores the need for deeper investigation into the intricate neurobiological connections between mood disorders and SUD, recognizing that these conditions may be linked by common genetic or environmental factors.
Substance use disorders (SUDs) and mental illnesses frequently coexist, a phenomenon known as comorbidity. Research consistently demonstrates a substantial overlap, with around half of individuals diagnosed with an SUD also meeting criteria for a mental health condition like depression or anxiety. This high rate of co-occurrence suggests a possible link between the underlying biological mechanisms driving these disorders.
It's hypothesized that shared brain pathways, particularly those involved in reward and stress responses, contribute to this overlap. In essence, the same biological changes that can lead to substance use might also increase susceptibility to mental health conditions. This idea is supported by the observation that individuals with both an SUD and a mental illness tend to experience a more severe course of each, with higher rates of treatment failure, relapse, and overall healthcare costs.
Further complicating matters, substance use can act as a temporary coping mechanism for individuals with mental health conditions, creating a cyclical pattern. Using substances might provide transient relief from anxiety or depression, inadvertently reinforcing the behavior and making it more challenging to discontinue use. Recognizing this interaction is critical, highlighting the need for treatment approaches that simultaneously address both the SUD and co-occurring mental health issue (dual diagnosis).
It's important to consider that certain substances may be more strongly associated with specific mental health disorders. For instance, while alcohol use often relates to depressive symptoms, stimulant use, such as cocaine, tends to be more closely linked with anxiety disorders. This relationship might be explained by how different drugs impact distinct neurotransmitter systems within the brain.
Furthermore, genetic factors play a prominent role in the comorbidity of these disorders. Studies suggest that individuals can inherit vulnerabilities that heighten the likelihood of developing both an SUD and a mental health condition, making treatment even more challenging. However, it's crucial to note that these genetic predispositions often interact with environmental factors to drive the development of these disorders.
Psychological factors like trauma and chronic stress can significantly contribute to the development of both SUDs and mental health disorders. These experiences can alter the brain's stress response systems, potentially increasing vulnerability to both types of conditions. Thus, addressing the impact of trauma or chronic stress is essential for effective intervention and treatment.
The brain regions affected by SUDs and mental illnesses can overlap, adding another layer of complexity to treatment. For example, the prefrontal cortex, a brain area crucial for decision-making, is frequently impacted in both conditions. This shared impairment can make it difficult for individuals to make rational choices about substance use, hindering their ability to engage in treatment or maintain abstinence.
It's notable that methamphetamine use, specifically, has been linked to higher rates of mental health issues, including psychosis and severe anxiety. This suggests that methamphetamine may disrupt neurotransmitter systems in a way that significantly increases risk for these conditions. Understanding the specific neurochemical changes caused by different drugs can be critical for tailoring effective treatment approaches.
Effective treatment for comorbid SUDs and mental health disorders frequently involves integrated approaches. These approaches often incorporate both medication and psychotherapy to comprehensively address both the SUD and the mental health condition. This highlights the need for a comprehensive understanding of how these disorders interact at the level of brain function and behavior to optimize treatment outcomes.
In summary, the comorbidity of SUDs and mental illnesses presents a significant challenge to treatment and prevention. The intricate interplay between biological, psychological, and environmental factors that contribute to both conditions emphasizes the need for multi-faceted and tailored approaches. Further research is needed to understand these relationships at a deeper level to develop the most effective prevention and treatment strategies and improve outcomes for individuals struggling with both disorders.
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Advancements in Neuroimaging for Predicting SUD Progression
Recent advancements in neuroimaging, particularly functional MRI (fMRI) and Event-Related Potentials (ERPs), have significantly enhanced our comprehension of how Substance Use Disorder (SUD) progresses. These techniques have revealed specific neural pathways, especially the corticostriatal circuits, that are central to both the development and relapse of addiction. While these discoveries are valuable, there's still a disconnect between the insights from neuroscience and their practical implementation in clinical settings. Clinicians are not routinely incorporating these neuroimaging-based understandings into treatment protocols, hindering the potential to improve treatment outcomes.
Current research is increasingly focusing on how the brain's capacity for change, neuroplasticity, interacts with addiction. This research hints that treatments specifically tailored to individual brain responses, as identified through neuroimaging, might lead to improved recovery rates. As we continue to develop our knowledge of addiction's neurobiological basis, bridging the gap between research findings and clinical practices is paramount. This will allow clinicians to leverage this understanding to enhance treatment and potentially improve the long-term prognosis for individuals grappling with SUD.
Substance Use Disorder (SUD) is a complex and chronic condition involving compulsive substance use despite negative consequences. Our understanding of the neurobiological underpinnings of SUD has greatly advanced due to neuroimaging techniques. These advancements have allowed us to pinpoint specific brain networks that play a role in addiction development and relapse, providing a window into the neurobiological factors that can predict or contribute to SUD progression.
Current theoretical frameworks of addiction suggest that dysfunction within the corticostriatal circuitry plays a central role in both vulnerability to and negative consequences of substance use. However, the gap between these findings and practical clinical application remains substantial, with limited adoption of neuroscience-informed interventions in treatment settings.
There's a growing interest in using Event-Related Potentials (ERPs) as potential biomarkers to track changes in behavior among individuals with SUDs. SUDs encompass a range of conditions, including alcohol use disorder, tobacco dependence, and dependence on substances like methamphetamine and heroin. Understanding the neurobiology of these different SUDs has led to an emphasis on developing more individualized treatment approaches that are tailored to the specific substance and the individual's unique brain activity patterns.
A major goal for the field is to bridge the gap between neuroscience discoveries and clinical practice. We need a clear roadmap for integrating neuroscience insights into addiction treatment protocols to enhance clinical effectiveness. Functional Magnetic Resonance Imaging (fMRI) has proven particularly useful in outlining both shared and distinct neural alterations across different SUDs, paving the way for more precise and targeted treatment strategies.
For instance, real-time fMRI monitoring allows us to see how cravings and triggers impact brain activity in individuals with SUD. Specific neural activity patterns, such as heightened activity in reward-related brain areas, are now being used as potential predictive biomarkers for SUD progression. This possibility raises intriguing prospects for early interventions to support individuals at high risk.
The integration of machine learning algorithms is enhancing our ability to analyze neuroimaging data, leading to more precise prediction of SUD outcomes based on individual brain activity patterns and personal histories. Surprisingly, even after prolonged substance use, brain regions such as the prefrontal cortex display evidence of neuroplasticity and recovery potential. This offers hope that specific treatment approaches might be able to promote brain healing.
Furthermore, neuroimaging has revealed how various substances produce unique changes in brain structure and function. For example, methamphetamine use shows distinctive alterations in the amygdala compared to alcohol dependence, supporting the need for distinct treatment strategies depending on the substance. We've also learned how substances affect the brain's stress response systems, often leading to increased activity in stress-related brain regions. This increased activity contributes to a cycle of addiction and stress that further complicates treatment.
Neuroimaging also gives us insights into how genetic predispositions are manifested in brain structures, highlighting the complex interplay of genetics and environmental factors in SUD development. Importantly, we've learned that some brain alterations related to SUDs can persist long after individuals stop using substances. This reinforces the idea that long-term support is crucial for recovery and relapse prevention.
Neuroimaging studies have also demonstrated significant alterations in the functional connectivity within brain networks associated with decision-making and impulse control in those with SUDs. This adds another layer of complexity to our understanding of the recovery process. Emerging research is finding connections between SUD and other disorders, suggesting that abnormalities in the brain's reward systems might be a common pathway underlying both SUD and mental health conditions. These insights could lead to the development of integrated treatment approaches that address both types of conditions simultaneously.
In conclusion, neuroimaging has greatly improved our understanding of the neurobiology of SUD. Continued research into the mechanisms of SUD, the predictive value of neuroimaging data, and the implementation of these findings into clinical practice are essential for developing more effective treatments, improving recovery outcomes, and preventing relapse.
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Integrating Pharmacological and Psychosocial Treatments
Successfully treating Substance Use Disorders (SUD) often necessitates a combined approach using both medication and psychosocial therapies. Pharmacological interventions, particularly for conditions like alcohol or opioid use disorder, can offer crucial support during withdrawal or management of cravings. However, their effectiveness is frequently enhanced when combined with psychosocial therapies. These therapies address the psychological, emotional, and social components that contribute to the development and maintenance of addictive behaviors.
Despite significant progress in understanding the brain changes linked to SUD, many clinicians haven't fully integrated these discoveries into routine practice. This highlights the ongoing need to bridge the gap between research findings and clinical application. Improving access to training and continuing education that emphasizes the neurobiological basis of addiction may be one strategy to achieve this.
Ultimately, a balanced approach that combines medical treatments and evidence-based psychosocial interventions is likely to provide the best chance of long-term recovery. This strategy holds the most promise for individuals with SUD to achieve lasting change and improve overall treatment outcomes.
1. **Combining Treatment Modalities**: Integrating pharmacological and psychosocial approaches has proven beneficial for individuals struggling with Substance Use Disorders (SUD). Research consistently shows that combining these methods yields better results than using either one alone, suggesting a potential for improved recovery outcomes.
2. **Developmental Impact**: When adolescents grapple with SUD, combining psychosocial therapies with any medication can help support their still-developing brains. Such a combination might help address specific cognitive deficits related to drug use, potentially enhancing areas like decision-making and other executive functions.
3. **Medication's Role**: Medications like buprenorphine, used for opioid use disorder, can be effective at reducing cravings. However, their impact is generally maximized when paired with behavioral therapies. These therapies help patients find motivation for recovery and manage the psychosocial factors that can trigger relapse.
4. **Shared Pathways in the Brain**: It's becoming increasingly clear that both pharmacological and psychosocial interventions may target similar neural systems, particularly those related to reward processing in the brain. This overlap hints at the potential for a synergistic treatment effect if carefully integrated.
5. **Sustained Recovery**: Evidence strongly suggests that people who participate in integrated treatment programs—combining both medication and therapy—are more likely to achieve and maintain long-term recovery compared to individuals who only receive one type of treatment.
6. **Preventing Relapse**: Studies show that incorporating cognitive-behavioral therapy alongside medication can effectively reduce relapse rates. This is particularly important during times of transition, for example, when a patient returns to a familiar, potentially high-risk environment after treatment.
7. **Real-Time Brain Feedback**: Researchers are exploring the use of new technologies that provide real-time brain feedback via neuroimaging. This approach aims to create treatment protocols that adapt in real-time, blending pharmacological and psychosocial approaches based on how an individual's brain reacts.
8. **Stress Response Management**: Psychosocial interventions can alter the brain's stress response systems. Techniques that help reduce stress, in conjunction with medication, could potentially lower relapse rates. The underlying idea is to improve emotional regulation and reduce overall vulnerability.
9. **A Chronic Condition Perspective**: Viewing SUD as a chronic disease requires a commitment to long-term treatment. This means incorporating psychosocial support into medication regimens as an ongoing aspect, rather than a one-time add-on. This integrated approach fosters continued engagement in recovery strategies over the long-term.
10. **Individual Variability**: It's important to acknowledge that combined treatments can have drastically different levels of success for different individuals, due to various genetic and environmental factors. This suggests that understanding patient-specific traits is crucial for crafting customized treatment plans that maximize the effectiveness of the combination of pharmacological and psychosocial approaches.
The Neurobiological Basis of Substance Use Disorder Recent Findings and Implications for Treatment - Challenges in Applying the Disease Model of Addiction
Applying the Disease Model of Addiction (DMA) has faced hurdles, mainly due to its tendency to view addiction as a strictly predetermined condition. While this model highlights the importance of biological factors in substance use disorders (SUD), some researchers find it insufficient in encompassing the varied experiences of addiction and the significant role of social and environmental factors. The ongoing disagreement about the classification of SUDs, as evidenced by the contrasting perspectives of the DSM-5 and ICD-11, further illustrates the ongoing complexities within the field. Moreover, recent research into the neurobiology of addiction points toward the importance of individual learning processes and unique circumstances, suggesting that treatment approaches should be more personalized. These challenges underscore the need for a more comprehensive understanding of addiction that blends the latest neuroscientific discoveries with an awareness of the intricate interplay between individual experiences and environmental influences.
1. **The Limited Scope of the Disease Model:** While the disease model of addiction, popularized by Alan Leshner, has been influential in framing addiction as a chronic brain condition characterized by compulsive drug-seeking, it sometimes oversimplifies the complex nature of addiction. It primarily focuses on the neurobiological aspects, potentially overlooking the crucial roles of psychosocial factors and individual choices in the development and maintenance of substance use disorders. This can limit the creation of holistic treatment plans that effectively address all the contributors to addiction.
2. **A Gap Between Research and Practice:** Despite significant advancements in neuroimaging, which has revealed considerable changes in brain structure and function associated with addiction, many clinicians haven't fully integrated these findings into their treatment approaches. This disconnect hinders the development of personalized treatment strategies informed by specific neurobiological insights from things like fMRI. This highlights the need for improved training and education for clinicians to bridge the gap between scientific discoveries and practical application in patient care.
3. **The Changeable Nature of Recovery:** Many individuals recovering from substance use disorders experience persistent alterations in brain structure and function. This perspective suggests that viewing addiction solely as a disease, with a clear path to recovery, might be overly simplistic. Some brain changes can remain even after abstinence, which indicates that long-term treatment and adaptable approaches are likely necessary for maintaining recovery. This is in contrast to a rigid, fixed disease model.
4. **Potential for Increased Stigma:** By solely categorizing addiction as a brain disease, there's a potential risk of perpetuating stigma and negative societal perceptions of individuals with substance use disorders. This can discourage individuals from seeking help, hindering access to treatment and support. This brings up an important discussion on the language we use when describing addiction and the impact of framing it in a particular way.
5. **Genetic Diversity in Addiction Response:** Individuals possess diverse genetic predispositions that influence their susceptibility to addiction and can affect their response to various treatments. This variability emphasizes the need for individualized treatment plans that take into account these genetic differences. While a disease model can be helpful, this variation makes a one-size-fits-all approach unlikely to be the most effective.
6. **The Significance of Early Intervention**: Exposure to drugs during adolescence can result in lasting neurobiological changes that pose challenges for later recovery. This finding underscores the importance of preventive strategies, especially targeting young people who might be at heightened risk of developing addiction. Prevention and very early intervention, especially with at risk individuals, might be one of the most effective long term approaches for reducing the prevalence of SUD.
7. **The Complexity of Co-occurring Disorders**: Individuals with substance use disorders frequently have comorbid mental health conditions, further complicating the picture. A narrow disease model that focuses solely on substance use might overlook the need for integrated treatment strategies addressing both the substance use disorder and the co-occurring mental health concerns. Integrated, patient specific, therapies might be more effective than therapies focused on solely treating the SUD.
8. **Cognitive Impairments and Treatment Challenges**: Substance use can lead to cognitive deficits, especially in decision-making and impulse control, due to changes in brain regions involved in these functions. These impairments can hinder the effectiveness of treatment interventions. Treatment interventions need to account for the various impacts on cognition caused by SUD.
9. **The Limitations of Neuroimaging:** While neuroimaging has provided invaluable insights into brain changes in addiction, the specific implications of these changes are still under investigation. The way different substances influence various brain regions can vary greatly. We need to develop better biomarkers and a more detailed understanding of exactly how these changes impact treatment outcomes.
10. **A Need for Evolving Treatment Models:** The understanding of addiction continues to evolve. This ongoing evolution raises questions about the continued applicability and sufficiency of the traditional disease model. Exploring other models that incorporate biological, psychological, and social factors might lead to more effective treatment strategies and enhanced long-term recovery outcomes. A more integrated, holistic approach, might be better than one focused solely on neurobiology.
More Posts from psychprofile.io:
- →How Sleep Deprivation Triggers Anxiety Attacks A Neurological Perspective
- →The Role of Digital Tools and AI-Powered Apps in Adult ADHD Management A 2024 Analysis
- →Breaking the Cycle How Negativity Bias Shapes Our Perception of Recurring Bad Events
- →Understanding the Bodily Impact of Panic Attacks
- →Childhood Trauma and Its Long-Term Impact on Anxiety Disorder Development
- →Childhood Abandonment and Its Long-Term Impact on Adult Anxiety New Research Findings from 2024