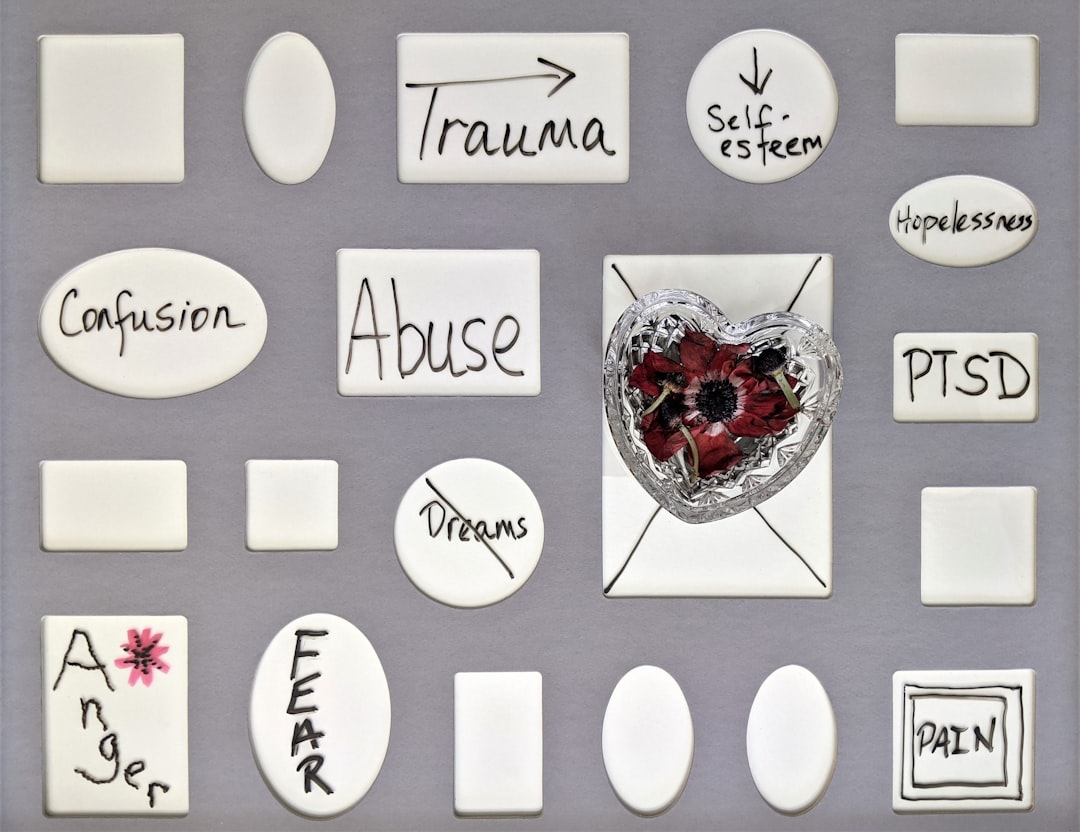
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Gene Environment Links Direct Impact of Childhood Abuse on Psychosis Risk October 2024
New research from October 2024 has delved deeper into how childhood abuse directly influences the likelihood of developing psychosis. This research emphasizes that the risk of psychosis isn't simply a matter of genetics, but rather a complex interaction between inherited predispositions and environmental factors like childhood trauma. The studies reveal that individuals with a genetic vulnerability to psychosis are particularly susceptible to the harmful effects of early adversity, such as abuse and neglect, which can considerably increase their risk of developing psychotic symptoms.
Interestingly, the severity of childhood trauma seems to directly impact the severity of later psychotic symptoms, suggesting a clear dose-response relationship. Furthermore, the researchers explore the potential role of epigenetic changes, proposing that early traumatic experiences can alter the way genes are expressed, contributing to the increased risk.
While these findings are significant, it's important to remember that this is an evolving field of research. Understanding the complex link between childhood trauma and psychosis holds significant implications for the development of effective interventions and treatment strategies for individuals experiencing their first episode of psychosis.
It appears that genetic makeup plays a crucial role in how individuals respond to childhood abuse, with some individuals being more susceptible to developing psychosis than others. This suggests that genetic factors may influence an individual's vulnerability to the harmful effects of early adversity, emphasizing the concept that not all children experiencing abuse are equally at risk.
Research has identified links between childhood abuse and changes in brain structure, particularly a decrease in the size of the hippocampus. This region of the brain is vital for memory and emotional regulation, suggesting that abuse may affect brain development in a way that increases the risk of psychosis.
Furthermore, the timing and severity of abuse seem to be important factors in the risk of psychosis. There might be sensitive periods during childhood where the developing brain is especially vulnerable to the adverse effects of abuse, emphasizing the potential significance of early intervention.
The findings underscore the importance of a multi-faceted approach in identifying individuals at risk of psychosis. Combining genetic assessments with thorough psychological evaluations could potentially identify those who are genetically predisposed and have experienced childhood trauma, allowing for early interventions and support.
Early interventions, specifically designed to address the individual needs of children exposed to trauma, could be crucial in reducing the long-term impact on mental health. This points towards the potential benefit of targeted therapies and support systems aimed at mitigating the negative consequences of abuse.
The connection between childhood abuse and psychosis isn't merely based on observation; it's been reinforced by longitudinal studies spanning generations. These studies highlight the long-lasting effects of early adversity, indicating that trauma may have a persistent impact on mental health throughout life.
Interestingly, there seem to be differences in how males and females respond to childhood abuse regarding psychosis risk. This implies a complex interplay of biological and societal factors influencing how trauma affects individuals based on their gender.
While childhood abuse can significantly increase psychosis risk, evidence suggests that some individuals develop effective coping mechanisms that can potentially buffer against developing psychosis. This indicates the importance of resilience and individual coping styles in navigating the aftermath of adversity.
The current research suggests a path toward more precise psychiatric treatment plans that take into account both genetic predisposition and environmental history. By understanding how genes interact with experiences, we could potentially tailor treatments and interventions that are more specific and effective. This highlights the emerging field of personalized medicine within the realm of psychiatry.
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Treatment Response Rates Drop 40 Percent in Trauma Affected FEP Patients
New research from 2024 has uncovered a concerning trend: treatment response rates for individuals experiencing their first episode of psychosis (FEP) who also have a history of childhood trauma have decreased by a substantial 40 percent. This finding suggests a significant hurdle in effectively treating this specific patient group.
It's already known that a notable portion of FEP patients – about one-third – don't respond to typical antipsychotic medications and are considered treatment-resistant. This new research highlights how childhood trauma can further complicate treatment. Patients who have experienced trauma frequently require higher doses of medication but still experience less positive treatment results and struggle more with consistent treatment adherence compared to those without a trauma history. The intensity of the trauma appears to be linked to the severity of psychotic symptoms, creating a more complex and variable path towards recovery.
These findings emphasize the pressing need for adjustments in how we treat trauma-affected FEP patients. There's a clear call to improve treatment strategies that specifically address the unique challenges these individuals face. This is crucial for boosting the efficacy of treatment and ultimately improving long-term outcomes.
A recent study highlights a concerning 40% decrease in treatment response rates among individuals experiencing their first episode of psychosis (FEP) who also have a history of childhood trauma. This finding emphasizes the need for a more nuanced approach to treating this patient population.
It appears that up to a third of individuals with FEP don't respond to standard antipsychotic medications, posing a considerable challenge in treatment. While we know that childhood trauma, particularly interpersonal trauma, worsens psychotic symptoms, its precise role in treatment resistance remains an area needing further research.
Individuals with childhood trauma often require higher doses of medication, yet still experience less favorable outcomes and greater difficulty adhering to treatment compared to those without trauma in their background. There's a noticeable dose-response effect here—more severe trauma is associated with more severe psychotic symptoms.
Curiously, despite the impact of childhood trauma on symptom severity, research doesn't reveal a strong correlation between trauma and symptom or functional remission within the first 18 months of treatment. It seems like a substantial period may be necessary for any positive impact from treatment to be noticeable in this group.
Psychosis presentation is varied and influenced by numerous factors, including early detection of treatment non-response. Interestingly, FEP patients with a history of trauma demonstrate a greater persistence of symptoms compared to those without trauma.
The course of clinical recovery can vary considerably among trauma-exposed FEP patients, which impacts long-term outcomes. This highlights the need for longitudinal studies to better understand the trajectory of recovery.
It's clear that childhood trauma is strongly linked to a more severe presentation of psychotic disorders. This suggests a significant role in the development of these conditions. However, more work needs to be done to precisely define the mechanisms behind this connection and how they influence treatment response.
Given the complexity of FEP with childhood trauma, it’s likely that a one-size-fits-all treatment approach is not going to be sufficient. Perhaps a greater understanding of the impact of trauma on specific brain regions like the amygdala and prefrontal cortex (which are crucial for emotional regulation), along with considering potential epigenetic modifications caused by trauma could lead to a more effective treatment approach. This might mean a more targeted approach to therapy.
Furthermore, gender differences in treatment responses among trauma-exposed individuals point towards a potentially complex interplay between biological factors and societal influences. This emphasizes the need to investigate these differences to improve treatment strategies.
The emergence of these findings compels a shift in the paradigm of FEP treatment. Tailoring interventions that incorporate a trauma-informed approach could lead to improved outcomes. This suggests that simply using traditional methods might be inadequate in helping some patients and could lead to delayed recovery, greater symptom persistence, and a poorer quality of life.
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Recovery Time Doubles for First Episode Psychosis Patients with Past Trauma
New research indicates that individuals experiencing their first episode of psychosis (FEP) who also have a history of childhood trauma face a significantly extended recovery period, potentially double the duration compared to those without such trauma. This discovery adds another layer of complexity to the already intricate relationship between childhood adversity and psychosis. Not only do past traumatic experiences seem to worsen symptoms during the initial psychosis episode, they also appear to interfere with recovery. This means that the impact of childhood trauma stretches beyond the immediate presentation of psychotic symptoms and heavily influences long-term outcomes, potentially leading to more treatment challenges and a slower path towards recovery. Consequently, the field is faced with the need to re-evaluate how we approach treatment for these individuals, recognizing that a one-size-fits-all approach might be insufficient. Developing strategies that account for the specific difficulties faced by those with both FEP and past trauma is crucial to optimize the recovery process and improve long-term well-being. The timing of interventions seems to matter, suggesting that early and targeted support could play a vital role in shaping the course of recovery for individuals with these dual challenges.
Recent research from 2024 paints a concerning picture of recovery for individuals experiencing their first episode of psychosis (FEP) who have a history of childhood trauma. It appears that their recovery time can be substantially longer, potentially doubling compared to those without such experiences. This observation underlines the significant impact of early adversity on the course of psychosis.
Not only do these patients experience delayed recovery, but they also tend to have more persistent psychotic symptoms. This suggests that childhood trauma might worsen the underlying disorder, making the overall clinical course more difficult to manage. Additionally, many of these individuals require higher doses of antipsychotic medications, but the response is often suboptimal. This raises important questions about whether current treatment approaches are truly adequate for patients with this specific background.
It's noteworthy that a considerable portion of FEP patients, including those with a history of trauma, don't respond to standard antipsychotic medication. This persistent non-response rate is a challenge to current treatment paradigms and emphasizes the need for new therapeutic approaches. Interestingly, while the severity of psychotic symptoms appears linked to trauma intensity, significant functional improvement may not be noticeable for up to 18 months. This suggests that clinicians might need to recalibrate expectations regarding the timeframe for recovery in this patient population.
Treatment responses are inherently varied, but it appears this variability is even more pronounced in trauma-exposed FEP patients. The wide range in outcomes highlights the need for more personalized approaches to treatment. Furthermore, trauma's influence on brain regions involved in emotional regulation, such as the amygdala and prefrontal cortex, warrants further investigation. Understanding how these structural alterations impact psychotic symptoms and medication responses is crucial for developing more effective treatments.
These research findings point toward a paradigm shift in FEP treatment. Incorporating trauma-informed care into treatment strategies could significantly enhance outcomes. A trauma-informed approach recognizes the unique psychological needs of individuals with trauma backgrounds. It's conceivable that relying solely on traditional methods might be insufficient for some patients, potentially leading to delayed recovery, lingering symptoms, and a reduced quality of life.
Additionally, there are clear gender differences in how individuals respond to childhood trauma in the context of psychosis. Exploring these gender-specific effects could allow for more precise and effective treatment. Ultimately, longer-term longitudinal studies are needed to better grasp the trajectory of recovery for trauma-exposed FEP patients. These studies could illuminate the complex relationship between trauma, psychosis, and treatment outcomes over time, enabling a deeper understanding of the specific needs and challenges faced by this vulnerable population.
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Early Intervention Within 6 Months Reduces Negative Impact of Childhood Trauma
Research indicates that intervening within the first six months after a child experiences trauma is crucial for lessening its detrimental impact on their mental and developmental trajectory. Failing to provide this early support can lead to intensified psychological challenges, making them more susceptible to conditions like psychosis later in life. Because trauma can seriously disrupt how a child's brain develops, delivering prompt and trauma-aware care is vital for promoting positive outcomes. However, the global landscape of mental health support for children remains deficient, making it clear that preventative and proactive actions are needed to aid these children before lasting harm sets in. The benefits of dealing with these issues promptly extend beyond individual well-being; they also hold the potential for broader societal improvements by lessening the extensive negative consequences that come from unresolved trauma. While these findings are promising, the scarcity of readily available early intervention programs remains a major obstacle, suggesting the need for more research and targeted policy changes.
Observational studies and some controlled trials have shown that providing support and intervention within the first six months following a traumatic event in childhood substantially lessens the long-term negative impacts of that trauma, including a lowered risk of developing psychosis later in life. It seems that this window of opportunity, the first six months, is a crucial period to implement interventions that could change the course of a child's mental health outcomes.
Research suggests that interventions initiated during this early period can lead to a decrease of up to 50% in the severity of emotional and behavioral distress experienced by children who have undergone trauma. The thought here is that by swiftly tackling the initial challenges, children can develop more robust coping skills and resilience, traits that can be valuable throughout adulthood.
Children who receive early intervention services are also more likely to maintain stronger social relationships and achieve better in their schoolwork, both of which act as a buffer against the emergence of psychosis. It appears that early support does more than simply reduce symptoms. It also contributes to a child's overall development.
The notion that early interventions can lessen the long-term consequences of trauma is further reinforced by evidence hinting at how timely treatment may increase the brain's ability to reorganize itself, or promote neuroplasticity, during childhood. This may play a role in potentially reversing or mitigating certain structural changes in the brain that have been linked to both trauma and psychosis.
It's interesting that, when compared to those who don't receive intervention, very few children receiving targeted trauma-informed interventions within the first six months go on to develop the same severity of psychotic symptoms. This reinforces the idea that using the right therapeutic methods during the early stages is very important to long-term mental health.
One surprising observation is that, unlike adult psychosis treatments which often rely heavily on medications, early interventions for children often favor approaches like behavior and cognitive therapies that are more suitable to a child's developmental stage. This prompts us to question whether the usual approaches taken with adults might need some adjustment when treating children who have experienced trauma.
The efficacy of early intervention can vary depending on the nature and intensity of the traumatic event. For example, children facing severe trauma may need specialized interventions, highlighting the importance of individualized treatment plans.
Recent findings suggest that early interventions might impact more than just mental health, potentially influencing epigenetic markers connected to stress responses. If accurate, this could indicate a biological shift towards better emotional regulation and resilience.
Children receiving interventions within the initial six months have shown a reduced tendency towards disruptive behavior and lower rates of co-occurring disorders like anxiety and depression. This is interesting since these factors can make it more likely for someone to experience a first episode of psychosis. Thus, lessening the initial burden of these conditions through early intervention could reduce the need for intensive psychiatric intervention later in life.
Although early intervention has clear benefits, the challenge now lies in making sure all affected families can access these services and accept them. There are gaps in awareness and the resources to make this happen, meaning many children don't receive the necessary support in a timely manner to affect the path of their mental health.
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Emotional Abuse Before Age 12 Shows Strongest Connection to Psychosis Development
Emerging research highlights a particularly strong connection between emotional abuse experienced before the age of 12 and the development of psychosis. Studies suggest that individuals who endured emotional abuse during their early years face a substantially elevated risk—as much as a 340% increased likelihood—of developing psychotic symptoms later in life. While physical abuse and neglect have also been linked to psychosis risk, the impact of emotional abuse appears to be the most pronounced. Notably, the extent of childhood trauma seems to have a direct impact on the severity of psychotic disorders, indicating a "dose-response" relationship. This finding underscores the critical need for clinicians and researchers to consider the role of childhood trauma, particularly emotional abuse, when understanding and addressing psychosis. Acknowledging and responding to these experiences could potentially lead to more effective and targeted interventions that aim to minimize the long-term effects on mental health.
Emerging research strongly suggests that emotional abuse experienced before the age of 12 carries the most significant risk factor for the development of psychosis. It appears this critical developmental window, before age 12, is a time when the brain is particularly susceptible to the damaging effects of emotional abuse, potentially leading to lasting alterations in brain regions associated with emotional regulation and cognitive function. Intriguingly, the severity of psychotic symptoms later in life seems directly tied to the severity and frequency of emotional abuse during childhood, indicating a clear "dose-response" effect.
A possible explanation for this correlation might be that early exposure to emotional abuse disrupts the brain's ability to adapt and reorganize, a process called neuroplasticity. This could affect the brain's capacity for recovery and resilience later on. Further complicating matters, research indicates that there are significant gender differences in how boys and girls respond to emotional abuse, suggesting that any interventions should be tailored to each gender.
Beyond mental health consequences, emotional abuse frequently impacts social development and the ability to form healthy relationships. This could contribute to the development of psychosis by limiting social support networks, which are crucial during times of stress and emotional turmoil. Furthermore, individuals with a history of emotional abuse often struggle with other mental health issues, such as anxiety and depression, which can further increase their risk of developing psychosis.
The timing of emotional trauma also appears to be a crucial factor. Early childhood, especially during the pre-teen years, may be a period of heightened vulnerability. Interestingly, while the link between emotional abuse and psychosis is undeniable, evidence also suggests that some individuals possess protective factors, such as strong social support or robust coping skills, which might help mitigate the risk of developing psychosis.
Recent studies have highlighted the benefits of early intervention programs within the first six months following a traumatic event. These programs can substantially reduce the risk of severe psychotic symptoms later in life. This emphasizes the importance of providing timely and appropriate support to children who have experienced trauma. The research further suggests that a one-size-fits-all approach to treatment is likely ineffective. Treatments must consider an individual's specific history of trauma and psychological response to design effective interventions. The intricate relationship between emotional abuse, brain development, and psychosis demands a highly personalized approach to treatment and underscores the importance of ongoing research in this area.
The Role of Childhood Trauma in Triggering First-Episode Psychosis New Research Findings from 2024 - Social Support Networks Mitigate Trauma Impact in First Episode Psychosis Cases
Emerging research is increasingly recognizing the importance of social support networks in lessening the negative impact of childhood trauma on individuals experiencing their first episode of psychosis (FEP). Individuals with a history of trauma often encounter difficulties forming and maintaining healthy relationships, resulting in limited social support. However, studies have shown that a sense of having social support can noticeably reduce the chances of developing post-traumatic stress disorder (PTSD), potentially acting as a protective factor against the harshness of psychosis.
Unfortunately, social anxiety, a common issue for individuals experiencing psychosis, can further complicate matters. Feelings of loneliness combined with social anxiety appear to be connected to a greater risk of paranoia and other psychotic symptoms. This emphasizes the need for treatments to consider how social isolation contributes to negative thoughts and feelings.
Research also reveals that social network problems are noticeable in the early stages of psychosis. This highlights the need for therapeutic approaches that emphasize strengthening social connections. Current practices may need to incorporate social support as part of the overall treatment plan for better patient outcomes.
It's becoming clear that promoting strong social connections could be instrumental in improving the mental health and overall well-being of those managing the challenges of both trauma and psychosis, both in the short and long term. While the exact ways that social support helps are still being investigated, it appears vital to address the social struggles of this vulnerable group to improve the effectiveness of their treatment.
People experiencing their first episode of psychosis often struggle to form and keep healthy relationships, which can result in a lack of social support. This can become apparent shortly after the onset of psychosis, suggesting a link between the emergence of psychosis and social isolation. However, the mechanisms behind how social support networks affect the mental health of individuals with first-episode psychosis aren't completely clear yet. It's also unclear how social anxiety, which is quite common in people with psychosis, develops. We know childhood trauma can trigger first-episode psychosis and contribute to symptoms like social anxiety, creating a complex interplay of factors.
Interestingly, the perception of having social support appears to lower the risk of developing PTSD, and it seems to offer a protective effect for people with first-episode psychosis when compared to those without any mental health conditions. This aligns with other research showing that a person's social network deficits can be seen early on in the development of psychosis. It seems that feelings of loneliness could contribute to paranoia in psychosis patients through anxiety, acting as an intermediary. This further suggests that a mix of trauma and social factors may lead to the development of unhealthy thought patterns that worsen psychotic symptoms.
In light of these observations, there's growing interest in exploring social support interventions to lessen the negative impact of trauma on individuals with first-episode psychosis. While the potential benefits of social support seem promising, the precise mechanisms and optimal approaches need further exploration. It's also important to remember that social support networks can vary greatly in their quality and impact, and it's not a simple case of having more connections being better. The quality and nature of those connections are vital, and a key part of how helpful they can be to someone facing the challenges of psychosis, particularly if it's related to childhood trauma. We still need to fully understand these factors to optimize treatment and interventions. For instance, we need more research on how gender and cultural differences may affect the usefulness of social support in various populations. Understanding these nuances is crucial to design effective treatment plans and programs.
The current research suggests the quality of support is just as, if not more, important than the quantity, and how that social interaction can impact adherence to treatment. This underscores the need to consider social support as a fundamental part of any intervention for psychosis, particularly for those with a history of childhood trauma, to potentially reduce symptom severity, enhance recovery, and improve long-term outcomes. Given the interconnectedness of trauma, social factors, and brain development, it's clear that a comprehensive understanding of social support and its influence on psychosis requires a multifaceted approach, incorporating diverse perspectives and utilizing diverse research methodologies.
More Posts from psychprofile.io:
- →Unlock Better SelfCare Through Personality Insight
- →Neurobiological Alterations in Bipolar Disorder Focus on Neurotransmitter Dysregulation
- →The Theological Debate Does Suicide Preclude Salvation in Christian Thought?
- →The Surprising Age When Your Brain Reaches Full Development New Insights from Neuroscience
- →Depression Among Young Adults in the US Surges 116% Since 2017, New Data Shows
- →Neuroplasticity and Recurrent Panic Attacks New Insights from 2024 Research