Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Neural Circuit Abnormalities in Emotion Regulation
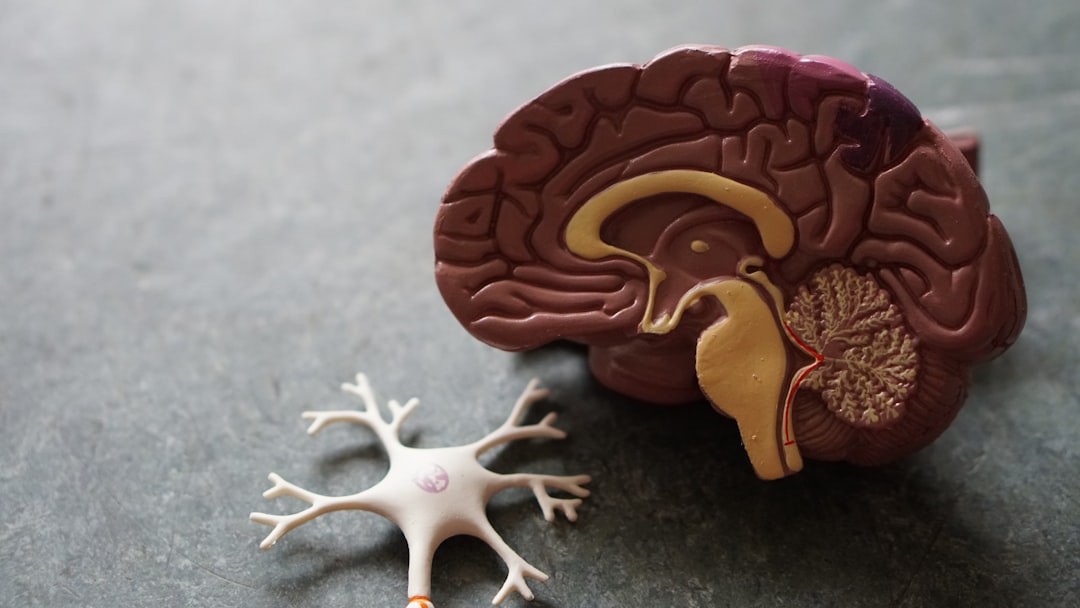
The intricate dance between brain regions is crucial for healthy emotional experiences, yet this delicate balance is disrupted in Borderline Personality Disorder (BPD). Individuals with BPD experience intense and erratic emotions, a hallmark of the disorder. These emotional difficulties arise, in part, from disruptions within the neural circuits governing emotional processing. Evidence suggests a key imbalance: prefrontal regions, typically involved in controlling emotions, appear to be less effective in regulating the activity of limbic areas, which generate emotional responses. This imbalance contributes to the pervasive emotional dysregulation seen in BPD. Notably, abnormalities within these circuits are observable even in adolescence, hinting at early developmental origins of emotional difficulties in this disorder.
Emerging research, using sophisticated neuroimaging techniques, is highlighting specific brain regions involved in this dysfunctional emotional processing. This new understanding of neural pathways offers a window into the core nature of emotional disturbances not only in BPD but potentially in other mental health conditions as well. Ultimately, a deeper understanding of these neural circuit irregularities may translate into better targeted therapeutic approaches, potentially enhancing outcomes for BPD treatment.
The amygdala, a brain region central to emotional processing, appears to be overly active in individuals with BPD, potentially leading to amplified emotional reactions compared to individuals without the disorder. Studies suggest that BPD might be associated with weakened communication between the prefrontal cortex, involved in higher-level cognitive functions like decision-making, and limbic areas governing emotional responses. This diminished connectivity could explain the challenges individuals with BPD face in effectively regulating their emotions, often manifesting as impulsivity and emotional volatility.
Further research points towards anomalies in the insula, a brain region vital for self-awareness and emotional experience. These abnormalities hint at a possible disconnect between emotional understanding and behavioral control in individuals with BPD. The dopamine system, traditionally implicated in reward processing and motivation, has also garnered attention in relation to BPD. Evidence suggests alterations in dopamine receptor function, potentially contributing to the instability in mood and heightened sensitivity to rewards often observed in these individuals.
Neuroimaging research has shown atypical activation patterns within the anterior cingulate cortex (ACC), a brain region crucial for emotional regulation and decision-making. This finding suggests the ACC's role in the difficulties experienced by those with BPD in managing their emotional responses and making choices. Structural analyses of the brain have revealed decreased volume in areas like the hippocampus, a structure crucial for memory and emotional processing. This reduction in volume could be linked to the pronounced emotional dysregulation seen in individuals with BPD.
The genetic underpinnings of neurotransmitter systems, specifically serotonin and norepinephrine, seem to be implicated in the observed neural circuit abnormalities related to emotional regulation. Furthermore, factors like inflammation and sensitivity to stress have been identified as potential biological contributors to the emotional dysregulation characteristic of BPD, suggesting a complex interaction between biological and environmental variables. Individuals with BPD often demonstrate heightened responses to stimuli that evoke fear and anxiety, indicating problems in effectively dampening negative emotions.
Recent research is beginning to explore the potential influence of traumatic experiences on the developing brains of individuals who later develop BPD. These findings propose that early adversity might significantly shape the neural circuitry underlying emotion regulation, potentially contributing to the vulnerability to BPD. This line of research suggests the intricate interplay between life experiences and the brain's developmental trajectories in the manifestation of BPD.
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Genetic Markers Linked to BPD Susceptibility
Research into Borderline Personality Disorder (BPD) is increasingly focusing on the role of genetics in its development. Evidence suggests that genetic factors play a substantial role alongside environmental influences like childhood trauma in shaping an individual's susceptibility to BPD. This means that a person's genetic makeup can contribute to their likelihood of developing the disorder. Scientists are diligently working to pinpoint specific genes or genetic variations that may increase the risk of BPD.
These investigations also explore how these genetic markers might relate to a broader understanding of personality disorders. Additionally, researchers are examining the intricate interplay between genes and environment through epigenetic patterns, which are changes in gene expression that are not directly related to the DNA sequence itself. Understanding this interplay is crucial for comprehending how genetic vulnerabilities can be influenced by life experiences and ultimately lead to the development of BPD.
The hope is that identifying these genetic factors will pave the way for a more comprehensive understanding of BPD, which could potentially lead to better diagnostic tools and treatment approaches for individuals struggling with this complex disorder. However, it is important to recognize the limitations of current knowledge and the need for ongoing research to clarify the intricate genetic and neurobiological underpinnings of BPD.
Borderline Personality Disorder (BPD) is increasingly understood to have a genetic component, alongside environmental influences. Research has begun to pinpoint specific genes that may contribute to a heightened susceptibility to developing BPD. Some of these genes influence the serotonin system, which plays a crucial role in mood regulation, suggesting a potential link between genetic variations and the emotional instability characteristic of BPD.
The brain-derived neurotrophic factor (BDNF) gene, involved in brain cell development and plasticity, has also been associated with BPD. Variations in this gene could impact an individual's resilience to stress, potentially affecting how they perceive and respond to emotional stimuli. The field is also exploring the role of epigenetics, where environmental factors influence gene expression without altering the DNA sequence itself. This could suggest that early life experiences can have long-lasting impacts on gene activity, ultimately affecting BPD risk.
Another area of interest is the link between genetics and inflammation. Certain genetic variations could contribute to heightened inflammatory responses, potentially exacerbating the emotional instability observed in BPD. The dopaminergic system, involved in reward and motivation, is also being investigated. Genes involved in regulating dopamine receptors have been associated with BPD, potentially influencing mood stability and impulsivity.
The catechol-O-methyltransferase (COMT) gene, which breaks down dopamine, has also been linked to BPD. This suggests a complex interaction between dopamine signaling and emotional regulation in BPD. Complicating matters further, several genetic markers linked to BPD are also associated with other mental health conditions, such as depression and anxiety. This overlap indicates a possible shared biological vulnerability across different disorders, making it challenging to identify specific genetic risk factors for BPD.
It's important to understand that genetic predispositions alone are not sufficient to explain the development of BPD. Environmental factors, such as childhood trauma, are also crucial in shaping an individual's vulnerability to the disorder. The interplay between these genetic and environmental factors remains a key area of investigation. A holistic understanding of BPD necessitates a multidisciplinary approach, combining genetics, neuroscience, and psychology to truly unravel the complexity of this disorder.
Excitingly, new technologies for genetic screening could one day allow for the identification of individuals at higher risk for BPD. This could potentially lead to early intervention strategies and more personalized therapeutic approaches, offering hope for improved outcomes. However, the path to understanding the complex interaction between genetics, environment, and brain function in BPD is still unfolding and will likely require years of further research.
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Neuroimaging Reveals Altered Amygdala Activity
Brain imaging techniques have unveiled a key characteristic of Borderline Personality Disorder (BPD): altered activity in the amygdala. The amygdala, a brain region vital for processing emotions, shows increased activity in those with BPD, possibly leading to amplified emotional reactions. This heightened amygdala activity, coupled with weakened communication between the amygdala and the prefrontal cortex (which helps control emotions), contributes to the difficulty regulating emotions often seen in BPD. Interestingly, this altered amygdala activity is now seen as a potential target for new therapies, including neurofeedback, aimed at improving emotion regulation. Continued research using these imaging methods is crucial to gain a deeper understanding of BPD's neural basis and potentially develop more effective treatment approaches.
Individuals with Borderline Personality Disorder (BPD) often display difficulties in managing emotions and understanding the emotional states of others. Neuroimaging techniques, particularly fMRI, have unearthed a compelling neurobiological aspect of BPD: altered amygdala activity. The amygdala, a key brain region for emotional processing, appears to function differently in individuals with BPD compared to those without.
This altered functionality doesn't simply mean heightened emotional reactions; instead, it suggests a heightened sensitivity to fear-related cues, which can impact social interactions and relationships significantly. There's evidence that this amygdala hyperactivity may be interconnected with impaired communication between the amygdala and the prefrontal cortex. This disrupted communication might explain why individuals with BPD often struggle with emotional regulation, leading to impulsivity and challenges managing emotional responses.
Interestingly, some of these alterations in amygdala activity are detectable in adolescents with BPD, highlighting the potential for early interventions to positively influence long-term emotional outcomes. Furthermore, stress appears to exacerbate the already elevated amygdala activity in these individuals. This observation underscores the crucial role of stress management strategies in therapeutic approaches for BPD.
Some research suggests that women with BPD might display even more pronounced amygdala hyperactivity than men, indicating a potential gender-specific aspect of the neurobiology of BPD. These altered amygdala patterns are possibly influenced by neurotransmitter systems, with the serotonin system potentially playing a key role in mood and emotional instability.
Beyond the extent of amygdala activity, the timing of its activation in response to emotional stimuli also seems abnormal in BPD. This suggests the importance of examining not only the strength of the response but also the temporal dynamics of amygdala activation during emotional experiences. Furthermore, consistent findings across a range of emotional stimuli—not just negative ones—suggest a broader issue in emotional processing in BPD.
Given the distinct patterns of amygdala activity observed through neuroimaging, researchers are beginning to explore whether these anomalies can serve as biomarkers for BPD diagnosis. This has the potential to refine current diagnostic criteria and improve our clinical understanding of this complex disorder. The research on the neurobiological aspects of BPD is still ongoing, yet this focus on the amygdala provides a valuable lens through which to understand the intricate and challenging emotional experiences of those living with BPD.
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Dysregulation of Stress Response Systems
The way stress impacts the body and mind, known as the stress response system, is significantly disrupted in individuals with Borderline Personality Disorder (BPD). People with BPD frequently show heightened sensitivity to stress, which can worsen their already existing emotional instability and impulsive behaviors. These reactions are connected to problems within the brain's natural systems that handle stress, affecting how individuals process information emotionally and cognitively. Scientific studies suggest that experiences of stress early in life might lead to changes in these systems, highlighting that both biological factors and a person's environment play a crucial role in BPD. By understanding this complex interplay, we can create treatments designed to help people with BPD develop better emotional regulation and increase their ability to cope with life's challenges.
The persistent experience of stress can disrupt the body's natural chemical processes for managing stress, primarily affecting the hypothalamic-pituitary-adrenal (HPA) axis. This system, which usually helps us adapt to challenging situations, can become overly sensitive in people with Borderline Personality Disorder (BPD). This oversensitivity contributes to their volatile mood swings and unstable emotional state.
Interestingly, individuals with BPD often have lower baseline levels of cortisol, a vital stress hormone. While this might seem counterintuitive, it can lead to either excessive or insufficient stress responses when faced with actual stressors. This peculiarity further complicates the difficulties in emotional regulation already present in BPD.
Research suggests that trauma—a common experience among those with BPD—can reshape the neural pathways responsible for managing stress. Essentially, it's like the brain's wiring gets altered, leading to heightened states of vigilance or anxiety even in the face of relatively minor stressors.
Another factor is the role of the autonomic nervous system, which controls our automatic responses to threats. In BPD, there seems to be a disturbance in the balance between the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) systems. This imbalance leads to an amplified 'fight-or-flight' reaction even in neutral situations, which is certainly not helpful for individuals already struggling with emotional instability.
Furthermore, a decrease in vagal tone—which impacts heart rate variability—is often observed in those with BPD. This reduced capacity for heart rate variability hints at a diminished ability to regulate emotions and adapt to stress.
The connection between the amygdala (involved in fear processing) and the prefrontal cortex (responsible for higher-level thinking and emotional control) is crucial for healthy emotional responses. However, in BPD, this interaction is often compromised by the persistent influence of stress. This disruption hinders accurate emotional assessment and appropriate emotional responses, perpetuating the cycle of difficulties in emotional regulation.
Remarkably, both inherited traits and environmental influences on gene expression (epigenetics) contribute to how our stress response system develops. Childhood trauma, for instance, can significantly alter the pathways associated with stress reactivity, influencing emotional wellbeing throughout life.
The notion of "allostatic load" represents the cumulative burden of chronic stress. In BPD, this load tends to be higher than usual, emphasizing the long-term consequences of maladaptive stress responses. These responses can contribute to a variety of physical and psychological issues.
Hormonal shifts associated with stress responses, such as those involving oxytocin and norepinephrine, show unusual patterns in BPD. These disruptions in hormone levels likely play a role in both social and emotional difficulties, hindering the ability to maintain healthy relationships, an area frequently challenged by those with BPD.
Promisingly, newer interventions like mindfulness and somatic experiencing therapies are showing some potential in helping people with BPD manage their dysregulated stress response. These therapies work by aiming to restructure the neural circuits associated with emotional processing and stress regulation. While there is still much to learn, these insights provide a valuable avenue for future research and could lead to improvements in the ways BPD is managed and treated.
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Impaired Social Cognition and Mentalization
Difficulties in social cognition and mentalization are increasingly understood as core aspects of Borderline Personality Disorder (BPD), significantly contributing to the interpersonal problems experienced by individuals with the disorder. These cognitive weaknesses impair the ability to understand and interpret the emotional and mental states of others, which, combined with the emotional dysregulation characteristic of BPD, exacerbate relationship difficulties. Although the extent of difficulties in recognizing emotions in individuals with BPD is still debated, there's widespread agreement that Theory of Mind—a critical skill for navigating social interactions—is notably impaired in BPD. This highlights the need for therapeutic approaches, such as mentalization-based therapy, that explicitly target these cognitive weaknesses. Mentalization-based therapy aims to help individuals with BPD better understand both their own and others' mental states within social situations. The link between social cognition difficulties and relational problems in BPD remains a significant research area, particularly in the context of the disorder's underlying neurobiology. Further research in this domain is needed to potentially improve treatments for BPD.
Difficulties in social understanding, a core aspect of Borderline Personality Disorder (BPD), involve a reduced capacity to decipher social cues, frequently leading to misinterpretations in relationships. This impairment seems connected to irregularities in brain areas like the amygdala and the medial prefrontal cortex, which are vital for processing emotions and social interactions.
Research hints at an intriguing paradox in BPD: individuals might be overly sensitive to nonverbal emotional cues like facial expressions, suggesting a heightened awareness of others' emotions. However, their ability to respond appropriately is often hindered due to weakened mentalization skills.
Mentalization, the ability to interpret our own and others' mental states, appears impaired in BPD. This dysfunction can contribute to persistent feelings of emptiness and the challenges in maintaining stable relationships, which are central to the emotional instability typical of the disorder.
Recently, a study highlighted that even when viewing neutral stimuli, individuals with BPD show unusual brain activity in the social cognition network. This suggests that social encounters are filtered through an active emotional lens, which can impede accurate perception of situations.
Brain imaging studies show that the connection between the amygdala and areas related to social cognition is often disrupted in BPD. This disrupted integration could potentially explain both the hypersensitivity to perceived social threats and the challenges in empathizing with others.
The intricate dance between impaired social cognition and emotional dysregulation in BPD can fuel a damaging cycle. Impulsive emotional responses can harm relationships, which can amplify feelings of abandonment and distress, escalating both emotional volatility and cognitive distortions about social interactions.
Interestingly, some research suggests that despite an overall impairment in mentalization, people with BPD might show intact or even improved abilities to mentalize during emotional crises. This implies that heightened emotional intensity can paradoxically sharpen their focus on others' mental states in certain situations.
Therapies aimed at social cognition, like Mentalization-Based Treatment (MBT), have shown positive results in BPD. These treatments aim to enhance individuals' capacity to comprehend their own and others' emotional and intentional states, which may alleviate the relational challenges common to the disorder.
The insula, a brain region vital for self-awareness and emotional processing, plays a fascinating role in the neurobiology of social cognition in BPD. Dysfunction in this area suggests that people with BPD might struggle to link their own emotional experiences to those of others, potentially complicating their social engagements.
Finally, researchers are investigating the potential of early interventions focused on developing social cognition in at-risk populations. Early detection and support could significantly lessen the long-term consequences of BPD, underscoring the need to address both the emotional and cognitive aspects of the disorder.
Unraveling the Neurobiological Underpinnings of Borderline Personality Disorder Latest Research Insights - Neurotransmitter Imbalances in BPD Pathophysiology
Neurotransmitter imbalances are increasingly recognized as a core element in the development and progression of Borderline Personality Disorder (BPD). These imbalances disrupt the delicate balance within the brain's communication systems, leading to the characteristic instability in emotions and behaviors seen in BPD. The serotonin and dopamine systems, which play crucial roles in mood and reward processing, appear to be particularly affected in individuals with BPD. This dysfunction can contribute to the experience of impulsive behaviors, intense emotional swings, and difficulty managing emotional responses.
Research is revealing a key role for NMDA neurotransmission in contributing to impulsive aggression and affective instability in BPD. This finding emphasizes that the interaction of genetic predispositions and environmental events like early trauma are important factors in the manifestation of BPD symptoms. Further research focusing on the intricate interplay between genetic markers and the neurochemical environment of individuals with BPD holds great promise in helping us understand the roots of this disorder and potentially refine treatment strategies. The understanding that both neurotransmitter function and individual life experiences work together to shape BPD indicates a need for a comprehensive and holistic approach in both research and clinical care. This complexity underscores the challenges and opportunities that remain in navigating the neurobiological landscape of BPD.
Borderline Personality Disorder (BPD) is increasingly understood to involve more than just serotonin imbalances in its neurobiology. Norepinephrine and GABA, vital for managing anxiety and stress responses, appear to play a significant role in the complex interplay affecting mood and emotional stability in BPD. For instance, individuals with BPD often show reduced GABAergic function, potentially contributing to heightened anxiety and emotional reactivity. Lower GABA levels could interfere with the brain's natural ability to dampen emotional responses.
The serotonin transporter gene (SLC6A4) has received considerable attention due to its link to emotional dysregulation in BPD. Variations in this gene might affect how serotonin is reabsorbed by the brain, potentially influencing mood stability and impulsivity. Research suggests that disturbed dopaminergic signaling could contribute to the impulsive behavior often observed in BPD. This alteration in dopamine pathways might cause an increased sensitivity to rewards and lead to impulsive decision-making, further challenging emotional regulation.
Inflammation may also be involved, with the presence of pro-inflammatory cytokines hinted at in individuals with BPD. This potential connection between inflammation and neurotransmitter imbalances raises questions about how inflammation might disrupt neurotransmitter signaling and amplify emotional dysregulation. While we typically associate stress with heightened cortisol, studies have identified unusual cortisol patterns in some individuals with BPD: low baseline cortisol coupled with exaggerated responses to stressors. This makes it difficult to understand the exact nature of stress physiology in BPD.
Genetic factors, such as polymorphisms linked to the brain-derived neurotrophic factor (BDNF) gene, seem to play a part in BPD by influencing neuroplasticity and, ultimately, emotional regulation. BDNF variations could affect the brain's capacity to adapt to emotional experiences. The timing of neurotransmitter release in response to stress can also be altered in BPD, potentially leading to variations in the intensity and duration of emotional responses, contributing to the unpredictable mood swings seen in the disorder.
Oxytocin, a peptide known for its role in social bonding and emotional regulation, has demonstrated varying levels in individuals with BPD, hinting at potential dysregulation in social-emotional contexts. This variability might disrupt the ability to form lasting interpersonal relationships. These complex neurobiological mechanisms, especially the intricate web of neurotransmitter imbalances, present considerable therapeutic challenges. Traditional approaches focused primarily on serotonin might be insufficient. It's conceivable that targeting a broader range of neurotransmitter systems could improve the effectiveness of BPD treatments and alleviate the challenges faced by those with this disorder.
More Posts from psychprofile.io:
- →Understanding the Lesser-Known Autonomic Symptoms in Panic Disorder A 2024 Clinical Perspective
- →Understanding Male Depression The Role of AI Profiling
- →Interpersonal and Social Rhythm Therapy (IPSRT) A Targeted Approach for Managing Bipolar Disorder
- →Esquizofrenia Comprendiendo los 7 Síntomas Clave y su Impacto en la Salud Mental
- →The Duration Dilemma Understanding the Typical Length of Bipolar Depressive Episodes
- →7 Hidden PTSD Warning Signs Beyond Flashbacks A Neurobiological Perspective